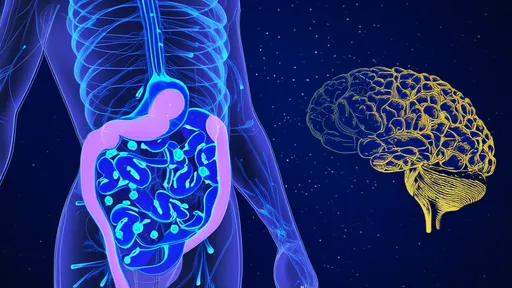
In the intricate landscape of human biology, few discoveries have captured scientific imagination like the gut-brain axis. For decades, this bidirectional communication highway between our digestive system and central nervous system has been a subject of intense research. Yet, recent breakthroughs have illuminated a fascinating new pathway that promises to revolutionize our understanding of mental health and neurological disorders. Scientists have uncovered compelling evidence that gut microbiota metabolites directly influence emotional states through the vagus nerve, creating what many are calling the most significant advancement in psychobiotic research this century.
The vagus nerve, that meandering cranial nerve stretching from brainstem to abdomen, has long been recognized as a critical information superhighway. But its role as the primary conduit for gut-derived emotional signals represents a paradigm shift in neurogastroenterology. Researchers at several leading institutions have demonstrated that specific microbial metabolites can stimulate vagal nerve endings in the gut lining, sending signals that directly modulate brain activity in regions governing mood, anxiety, and emotional response.
What makes this discovery particularly remarkable is the specificity of the communication. It's not merely general signals traveling upward, but targeted chemical messages that appear to influence very particular emotional states. The metabolites produced by certain bacterial strains have been shown to reduce anxiety-like behaviors in animal models, while others appear to enhance stress resilience. This precision suggests that our gut microbes might be actively participating in emotional regulation rather than merely influencing it indirectly.
The chemical messengers involved in this process represent a fascinating array of microbial metabolites. Short-chain fatty acids like butyrate, produced through bacterial fermentation of dietary fiber, have demonstrated remarkable effects on emotional centers in the brain. These compounds don't just passively diffuse into circulation; they actively engage with receptors on vagal nerve terminals, initiating signals that travel directly to the brainstem and beyond.
Other microbial metabolites including tryptophan derivatives, secondary bile acids, and various neuroactive compounds have joined the ranks of recognized gut-brain messengers. Each appears to play a distinct role in this sophisticated chemical dialogue. The implications are profound: the foods we eat don't just feed us; they feed our microbial partners who in turn produce compounds that shape our emotional landscape through direct neural signaling.
Human studies have begun to corroborate these mechanistic findings from laboratory research. Clinical trials involving probiotic interventions show changes not just in gut microbiome composition, but in actual brain activity patterns as measured by functional MRI. Participants receiving specific probiotic strains demonstrate altered emotional processing and reduced reactivity to negative stimuli, effects that correlate with changes in microbial metabolite profiles and vagal nerve tone measurements.
The therapeutic potential of these findings cannot be overstated. For the millions suffering from mood disorders, anxiety conditions, and treatment-resistant depression, this new understanding offers hope for novel intervention strategies. Rather than targeting brain chemistry directly through pharmaceuticals, we might eventually learn to modulate it through precision probiotics, targeted dietary interventions, or even vagus nerve stimulation techniques that acknowledge this gut-brain connection.
Perhaps most intriguing is the emerging evidence that this gut-vagus-brain pathway operates in both directions. Just as gut metabolites influence emotional states, emotional states appear to influence gut physiology through vagal feedback loops. This creates a fascinating biological dialogue where mental state and gut environment continuously inform and modify each other. The implications for conditions like irritable bowel syndrome, where stress and digestive symptoms intertwine, are particularly significant.
As research progresses, scientists are beginning to map the specific bacterial strains most involved in this emotional signaling. Certain Lactobacillus and Bifidobacterium species appear particularly potent in their ability to produce psychactive metabolites that engage the vagus nerve. Other less familiar microbial players are emerging as important contributors to this complex chemical conversation happening within us every moment.
The practical applications of this knowledge are already beginning to emerge. Nutritional psychiatry, once a fringe concept, is gaining mainstream traction as studies demonstrate that dietary patterns influencing microbiome composition correlate with mental health outcomes. The Mediterranean diet, rich in fiber and fermented foods, shows particular promise in supporting the microbial ecosystems that produce beneficial metabolites engaging the vagus nerve.
Yet challenges remain in translating these exciting discoveries into clinical practice. The incredible individuality of each person's microbiome creates complexity in developing universal interventions. What benefits one person's emotional health through this gut-vagus-brain pathway might have different effects in another individual with distinct microbial ecology. Personalization appears key to harnessing this knowledge effectively.
Future research directions are taking shape with remarkable speed. Scientists are exploring how to optimize microbial communities for mental health benefits, how dietary components can be tailored to support metabolite production, and how existing treatments might be enhanced by acknowledging this gut-brain connection. The emerging field of psychobiotics—live organisms that when ingested produce psychological benefits—stands poised for significant advancement based on these vagal nerve findings.
Beyond mental health, this research has implications for neurological conditions ranging from Parkinson's disease to autism spectrum disorders. Evidence suggests that the gut-brain communication pathway might be involved in much more than emotional regulation, potentially influencing neurodevelopment, neurodegenerative processes, and even cognitive function. The vagus nerve appears to serve as a central conduit in this expanded understanding of body-brain communication.
As we continue to unravel the complexities of this system, one thing becomes increasingly clear: the artificial separation between mental and physical health grows increasingly untenable. The gut-brain axis, particularly through this vagus nerve pathway, demonstrates the profound integration of our biological systems. Our emotional experiences are not just products of brain activity but emerge from a continuous dialogue between our nervous system, our digestive system, and the trillions of microbial partners we host.
This research doesn't diminish the importance of psychological factors or brain chemistry in mental health, but rather expands our understanding to include this crucial gut-brain communication pathway. It offers a more comprehensive, systems-level view of emotional health that acknowledges the multiple influences shaping our mental states. The implications for both treatment and prevention of mental health disorders are substantial and far-reaching.
For the scientific community, these findings represent both an achievement and a challenge. The achievement lies in uncovering this sophisticated communication system that operates beneath our awareness. The challenge lies in translating this knowledge into practical applications that respect the complexity of individual microbiomes while providing meaningful mental health benefits. The coming years will likely see accelerated research efforts aimed at meeting this challenge.
For the general public, these discoveries offer a new perspective on the mind-body connection—one grounded in cutting-edge science rather than vague philosophy. They provide biological explanations for why certain foods might influence mood, why gut health and mental health often intertwine, and why interventions targeting the digestive system might unexpectedly benefit emotional well-being. This knowledge empowers individuals to make informed choices about diet and lifestyle that support both physical and mental health.
The story of the gut-brain axis continues to unfold with increasing complexity and fascination. As we learn more about how microbial metabolites communicate with our brains through the vagus nerve, we gain not just scientific knowledge but practical insights into promoting mental well-being. This research stands as a testament to the incredible sophistication of human biology and the endless surprises it continues to reveal about the connections between different aspects of our health.

By /Aug 27, 2025
By /Aug 27, 2025
By /Aug 27, 2025

By /Aug 27, 2025

By /Aug 27, 2025
By /Aug 27, 2025

By /Aug 27, 2025

By /Aug 27, 2025
By /Aug 27, 2025
By /Aug 27, 2025
By /Aug 27, 2025

By /Aug 27, 2025

By /Aug 27, 2025

By /Aug 27, 2025

By /Aug 27, 2025
By /Aug 27, 2025
By /Aug 27, 2025

By /Aug 27, 2025

By /Aug 27, 2025
By /Aug 27, 2025