In the ever-evolving landscape of regenerative medicine, the quest to generate functional, mature cardiomyocytes through direct reprogramming has emerged as a groundbreaking frontier. This approach, known as direct transdifferentiation, bypasses the pluripotent stem cell stage, offering a potentially safer and more efficient route to cardiac cell therapy. Unlike traditional methods that rely on induced pluripotent stem cells (iPSCs), direct reprogramming converts somatic cells, such as fibroblasts, directly into cardiomyocytes, minimizing risks of tumorigenesis and ethical concerns. The implications for treating heart disease, the leading cause of death globally, are profound, as this technology could enable the repair of damaged heart tissue with patient-specific cells.
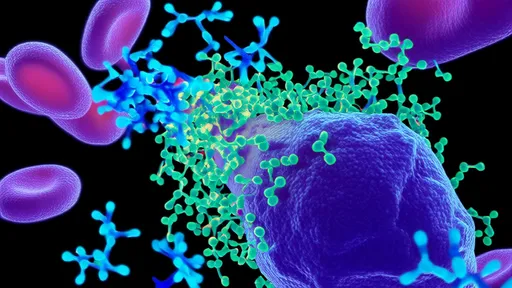
The concept of cellular reprogramming was revolutionized by the discovery that somatic cells could be reprogrammed to a pluripotent state through the introduction of specific transcription factors. Building on this foundation, scientists began exploring the possibility of directly converting one differentiated cell type into another without reverting to a pluripotent intermediate. In the context of cardiology, this meant transforming fibroblasts, which are abundant in scar tissue post-myocardial infarction, into functional cardiomyocytes. Early studies identified key transcription factors, such as Gata4, Mef2c, and Tbx5 (collectively known as GMT), that could initiate this process in vitro and in vivo.
Initial successes in direct cardiac reprogramming were met with enthusiasm, but also with challenges. The efficiency of conversion was low, and the resulting cells often exhibited immature characteristics, resembling fetal rather than adult cardiomyocytes. Functional maturity is critical for clinical application, as immature cells may not integrate properly into the host tissue or exhibit the necessary electrophysiological properties for synchronized contraction. Researchers have since focused on optimizing reprogramming protocols by incorporating additional factors, such as Hand2, microRNAs, and small molecules, to enhance efficiency and promote maturation.
One of the most significant advances has been the development of strategies to achieve greater functional maturity in directly reprogrammed cardiomyocytes. Mature cardiomyocytes are characterized by their rod-shaped morphology, organized sarcomeric structures, adult-like gene expression profiles, and the ability to generate forceful contractions. To induce these traits, scientists have employed various approaches, including prolonged culture periods, electrical stimulation, mechanical stretching, and co-culture with other cell types. These methods mimic the natural microenvironment of the heart, providing cues that guide the cells toward a more adult-like state.
Moreover, the use of epigenetic modifiers has proven instrumental in unlocking the full potential of direct reprogramming. Chromatin structure and DNA methylation patterns play a crucial role in cell identity, and altering these epigenetic landscapes can facilitate more stable and complete reprogramming. For instance, inhibitors of histone deacetylases (HDACs) or DNA methyltransferases (DNMTs) have been shown to improve reprogramming efficiency and promote the acquisition of mature features. This epigenetic insight has not only advanced the field but also highlighted the complexity of cellular identity and the barriers that must be overcome for successful transdifferentiation.
In vivo direct reprogramming represents another leap forward, offering the possibility of repairing damaged hearts without the need for cell transplantation. By delivering reprogramming factors directly to the heart via viral vectors or non-viral methods, researchers have successfully converted cardiac fibroblasts into cardiomyocyte-like cells in animal models of myocardial infarction. These newly formed cells integrate into the existing tissue, improve cardiac function, and reduce scarring. However, challenges remain, including controlling the specificity and safety of in vivo delivery, ensuring the long-term stability of reprogrammed cells, and avoiding unintended off-target effects.
The translational potential of directly reprogrammed cardiomyocytes is immense, but it must be navigated with caution. Clinical applications will require rigorous validation of safety, efficacy, and scalability. Key considerations include the choice of delivery vectors, the risk of immune responses, and the potential for arrhythmias due to heterogeneous cell populations. Additionally, manufacturing processes must be developed to produce large quantities of high-quality cells under Good Manufacturing Practice (GMP) conditions. Collaborative efforts between academia, industry, and regulatory bodies are essential to address these hurdles and move toward clinical trials.
Looking ahead, the future of direct cardiac reprogramming is bright, with ongoing research exploring novel factors, combination therapies, and personalized approaches. The integration of CRISPR-based gene editing could further refine reprogramming by precisely modulating gene expression or correcting mutations in patient-derived cells. Furthermore, understanding the mechanistic details of reprogramming at single-cell resolution may reveal new insights into cardiac development and disease. As these technologies mature, they hold the promise of transforming the treatment of heart failure, offering hope to millions of patients worldwide.
In conclusion, direct transdifferentiation to generate functional mature cardiomyocytes stands as a testament to the incredible progress in cellular reprogramming. While significant challenges remain, the advances made thus far underscore the potential of this approach to revolutionize cardiac regenerative medicine. By continuing to unravel the complexities of cell fate and maturation, scientists are paving the way for innovative therapies that could one day restore function to the damaged heart.

By /Aug 27, 2025
By /Aug 27, 2025
By /Aug 27, 2025

By /Aug 27, 2025

By /Aug 27, 2025
By /Aug 27, 2025

By /Aug 27, 2025

By /Aug 27, 2025
By /Aug 27, 2025
By /Aug 27, 2025
By /Aug 27, 2025

By /Aug 27, 2025

By /Aug 27, 2025

By /Aug 27, 2025

By /Aug 27, 2025
By /Aug 27, 2025
By /Aug 27, 2025

By /Aug 27, 2025

By /Aug 27, 2025
By /Aug 27, 2025