In a groundbreaking development that could reshape our approach to aging and age-related diseases, scientists have unveiled a novel strategy using engineered CAR-T cells to selectively eliminate senescent cells from the body. This innovative approach harnesses the precision of immunotherapy to target one of the fundamental drivers of biological aging, opening new avenues for therapeutic interventions.
Senescent cells, which accumulate with age, are cells that have stopped dividing but resist apoptosis. While initially beneficial in processes like wound healing and tumor suppression, their persistent presence contributes to chronic inflammation, tissue dysfunction, and the progression of numerous age-related pathologies. The quest to clear these cells, a field known as senolysis, has gained significant momentum over the past decade. Traditional small-molecule senolytics have shown promise but often lack specificity and can produce off-target effects. The advent of CAR-T cell therapy, a form of immunotherapy that has revolutionized cancer treatment, offers a remarkably precise and potent alternative for targeting these problematic cells.
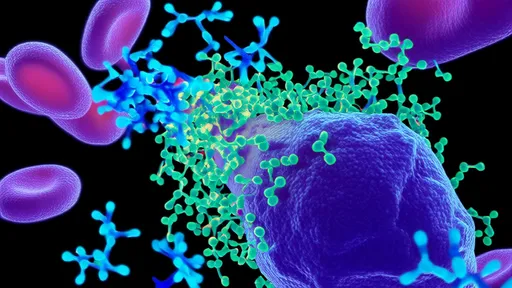
The core principle behind this new strategy involves genetically engineering a patient's own T cells to express chimeric antigen receptors (CARs) that are designed to recognize specific surface proteins unique to senescent cells. Much like how CAR-T cells are directed to hunt cancer cells, these senolytic CAR-T cells are programmed to seek out, bind to, and destroy senescent cells with high specificity. This method leverages the immune system's natural killing machinery, providing a powerful and potentially long-lasting effect against cellular senescence.
Early preclinical research, primarily in mouse models, has yielded exceptionally encouraging results. Studies have demonstrated that a single administration of these specially designed CAR-T cells can effectively reduce the burden of senescent cells in various tissues, including the liver, lungs, and fat. Consequently, treated animals have shown significant improvements in health metrics, such as enhanced metabolic function, increased physical endurance, and a reduction in biomarkers associated with inflammation. Perhaps most strikingly, these interventions have extended the healthspan—the period of life spent in good health—of the animal models, suggesting a direct impact on the aging process itself.
The potential therapeutic applications of this technology are vast. It could be deployed to treat a wide spectrum of conditions where senescent cells play a causative role. This includes fibrotic diseases like idiopathic pulmonary fibrosis and liver fibrosis, metabolic disorders such as type 2 diabetes, neurodegenerative conditions including Alzheimer's disease, and even osteoarthritis. By clearing the inflammatory senescent cells that drive tissue degeneration, this therapy could halt or even reverse the progression of these debilitating illnesses, offering hope to millions of patients for whom treatment options are currently limited.
Despite the exciting promise, the translation of senolytic CAR-T therapy to human clinics is not without its challenges. A primary concern is ensuring absolute specificity to avoid the unintended destruction of healthy, non-senescent cells that might express low levels of the target antigen. Researchers are actively investigating a suite of novel surface markers that are highly and exclusively expressed on senescent cells to serve as optimal targets for the CAR constructs. Furthermore, the safety profile of CAR-T cells, known for potentially severe side effects like cytokine release syndrome (CRS) in cancer therapy, must be carefully managed in a context where the patients may be older and more frail. Strategies such as incorporating "safety switches" that allow clinicians to deactivate the engineered cells if necessary are a critical area of development.
The journey from laboratory breakthroughs to a widely available treatment will be a meticulous one. Following the compelling preclinical data, the next crucial steps will involve rigorous testing in human clinical trials. These trials will need to carefully evaluate the therapy's efficacy, optimal dosing, long-term safety, and durability of response. The scientific and medical communities are watching this space with great anticipation, aware that success could herald a new chapter in medicine—one where aging itself becomes a modifiable condition.
In conclusion, the fusion of senolytic science and cutting-edge CAR-T cell technology represents a paradigm shift in our ability to combat the diseases of aging. This strategy moves beyond merely managing symptoms to addressing a root cause of age-related decline. While hurdles remain, the prospect of using our body's own engineered immune cells to purge it of senescent cells and restore function is a powerful and inspiring vision for the future of medicine and human health.

By /Aug 27, 2025
By /Aug 27, 2025
By /Aug 27, 2025

By /Aug 27, 2025

By /Aug 27, 2025
By /Aug 27, 2025

By /Aug 27, 2025

By /Aug 27, 2025
By /Aug 27, 2025
By /Aug 27, 2025
By /Aug 27, 2025

By /Aug 27, 2025

By /Aug 27, 2025

By /Aug 27, 2025

By /Aug 27, 2025
By /Aug 27, 2025
By /Aug 27, 2025

By /Aug 27, 2025

By /Aug 27, 2025
By /Aug 27, 2025